Dental Implants
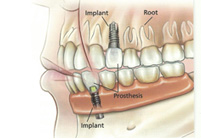 Dental implants (artificial teeth) may be used in people who have missing teeth. Dental implant techniques range from replacing one missing tooth to replacing most teeth in the upper and lower jaws. Dental implants have become a significant part of modern dentistry and millions of people around the world have had a variety of implants. The basic structure consists of the implant fixture and the prosthesis.
Dental implants (artificial teeth) may be used in people who have missing teeth. Dental implant techniques range from replacing one missing tooth to replacing most teeth in the upper and lower jaws. Dental implants have become a significant part of modern dentistry and millions of people around the world have had a variety of implants. The basic structure consists of the implant fixture and the prosthesis.
Implant
An implant fixture is inserted into the jaw bone to provide a base for supporting and attaching the prosthesis.
Prosthesis
A prosthesis, is an artificial tooth, or row of artificial teeth attached to the implant. The prosthesis may be a “crown” to replace one absent tooth or a “bridge” to replace several absent teeth. In a jaw with no teeth present, the prosthesis covers almost the full dental arch. Some prostheses with many teeth are fixed permanently onto the implants with screws or special cement. Other types of prostheses can be taken out for daily cleaning. These are called “over-dentures”.
Implant designs, materials and techniques have improved significantly over the past 20 years and are continuing to advance. Many different types of implants and prostheses are available for people with diverse needs. Implants may be manufactured with different materials and implanted using various methods. Each has its own advantages and disadvantages, and your surgeon will discuss which implant system best suits your requirements.
Why Dental Implants Are Beneficial
Implants provide points of fixed attachment for dental prostheses, and can help resolve problems posed by traditional dentures and bridges. Many people have described that dental implants are more comfortable, convenient and attractive than the dentures they had previously worn. They also report fewer difficulties when eating and talking. Biting and chewing are often very similar to biting and chewing with normal teeth.
In order to get bridges to fit correctly, adjacent healthy teeth need to be cut and reshaped which damages them. In contrast, adjacent natural teeth do not have to be altered or damaged when implants are used.
Bonding of the implant and jaw bone
Implants are made of materials (such as metal titanium) that can bond strongly to bone tissue. The bone tissue grows onto the surface of the implant. This is referred to as “osseointegration” and “biointegration”. You may hear your surgeon use these terms. When an implant is fixed securely to the jaw bone it can withstand the daily forces of chewing and normal function.
Who May Benefit From Implants
- Young people
Oral and maxillofacial surgeons and prosthodontists generally recommend a minimum age of 18 or 20 when bone growth has ceased. - Adults
Implants have been successfully used in adults of all ages including the elderly. - Chronically ill people
Some people with chronic illness find it quite difficult to chew food with dentures. Implants may be a more beneficial option.
Patient selection
To ensure that a person fully understands the requirements and benefits of completing their course of treatment, your surgeon will carry out a thorough examination and discussion with you.
The Decision To Have Implants
Following a consultation and examination, your surgeon will discuss whether you are likely to benefit from dental implants. The decision to undergo dental implant surgery is always yours, and you should not be pressured by anyone. If you decide to have implants, your surgeon will ask you to sign a consent form. You will need to read this carefully and if you have any questions or concerns regarding the implant surgery, ask your surgeon.
Your Dental And Medical History
Your surgeon will discuss your medical history and any dental or general health problems you may have. It is important to inform your surgeon of any health issues, and medications you are currently taking or have recently been taking. Your surgeon needs to be aware of this information as some health problems may interfere with the implant surgery, anaesthesia and post-operative care. This information assists your surgeon in planning the best possible treatment for you.
Tell your surgeon if you have:
- had any excessive bleeding problems when you were injured or had surgery
- any blood disorders, such as haemophilia
- had heart surgery
- had radiotherapy to your face or jaws
- had any problems with previous dental implant treatment
- osteoporosis and are having treatment for it
- any condition requiring long term steroid treatment
Medicines
Give your surgeon a list of all medications you are taking now or have been taking recently. This includes any bisphosphonate medication (taken for osteoporosis or other bone conditions), the contraceptive pill or any over-the-counter medications, such as aspirin or cough medicine.
When Implant Therapy Should Not Be Undertaken
Some people should not have or should delay having implants for the following reasons:
- Unrealistic expectations. A realistic outlook is important. Implant therapy is not successful for everyone. Some reconstructions can be very difficult, and the results may not be as good as the patient had envisaged.
- Pregnancy: Inform your surgeon if you are or may be pregnant. General anaesthesia is likely to an unnecessary risk for the mother and baby. Pregnancy could affect treatment with pain medications, antibiotics and other medicines. Pregnant women should wait until they have given birth before commencing implant therapy.
- Chronic illness: People with a chronic illness may not be able to tolerate general anaesthesia and may be unable to maintain the oral hygiene required for implants.
- Inadequate jaw bone. If too much jaw bone has been lost due to ageing and extraction of teeth, the implant will not adequate bone to secure it (see “Bone grafts and regeneration”, below).
- Any conditions, diseases or treatment that may hinder the healing process.
- Inability to maintain adequate oral hygiene.
- Psychiatric conditions: Some disorders may affect the ability to understand and comply with all the instructions.
- Drug and alcohol abuse: These may interfere with good nutrition, ability to follow the surgeon’s advice, maintenance of oral hygiene, and healing and osseointegration of the implant.
- Bisphosphonate therapy: Bisphosphonates reduce bone turnover so implants may fail to integrate and subsequently may lose integration. The risk is low with oral bisphosphonates (about 1%) but high with intravenous bisphosphonates (about 15%).
Bone grafts and regeneration
In some patients, bone may need to be grafted onto the jaw bone. The grafts will provide additional bone to support the implants. The bone is generally taken from another part of the jaw or from the hip. In patients who do not have enough bone in the jaw, more bone can be encouraged to grow using a method called “guided-tissue regeneration”. If you require bone grafts or guided-tissue regeneration, your surgeon will discuss this in detail with you.
Smoking
Your surgeon may decline to treat you if you continue to smoke. Smoking can precipitate failure of the implant to bond with the jaw bone. Smoking can significantly increase the risk of failure. To improve the chances of success, it is important that you cease smoking.
Implant Surgery
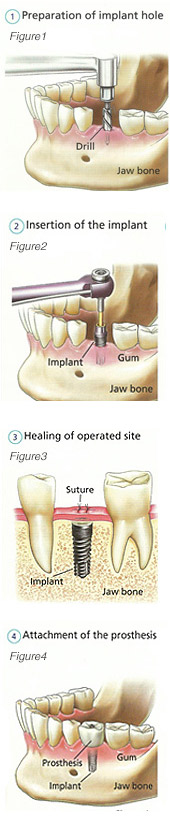 Your surgeon will make an incision to open your gums figure 1. The implant is then inserted into the jaw bone using special techniques and instruments figure 2. Different types of implants have been developed and not all are inserted into the bone. Your surgeon will discuss with you what type of implant system is best suited to your needs. The number of implants inserted by your surgeon depends on the prosthesis. For instance, one implant is used for replacing one absent tooth, or for a complete upper prosthesis having 12 artificial teeth, six or more implants may be required.
Your surgeon will make an incision to open your gums figure 1. The implant is then inserted into the jaw bone using special techniques and instruments figure 2. Different types of implants have been developed and not all are inserted into the bone. Your surgeon will discuss with you what type of implant system is best suited to your needs. The number of implants inserted by your surgeon depends on the prosthesis. For instance, one implant is used for replacing one absent tooth, or for a complete upper prosthesis having 12 artificial teeth, six or more implants may be required.
Once the implant has been inserted, the incision area is closed with stitches figure 3. Some stitches are self-dissolving after a few days, and other stitches require removal by your surgeon. The bone surrounding the implant is allowed to heal for up to three to six months.
Insertion of abutments – if not inserted at the time of your implant surgery
An “abutment” is inserted through the gums and into the implant. This can be done under a local anaesthetic. The abutment is the anchorage, support or connector for the prosthesis. The gums around the abutments are left to heal for several weeks.
Fitting the prosthesis
Your surgeon, prosthodontist or dentist will examine the implants to see if they have integrated with the bone. The implants must be strong enough to support the prosthesis and withstand the forces of chewing and normal function. If the implants have been successful, your prosthodontist or dentist will begin work on the prosthesis figure 4. The prosthesis may be fixed to the implant with cement or screws so that it is not removable. It may also be attached in a way that allows it to be removed for cleaning. These are called “overdentures”. When the impressions of your mouth are prepared and before the prosthesis is finished, discuss the aesthetics of the prosthesis with your dentist or prosthodontist. If you have any questions or concerns regarding the appearance of your prosthesis, discuss them with your dentist or prosthodontist.
Single-stage procedure
Some surgeons prefer to use a single-stage procedure, where the abutment and prosthesis are placed at the same time as the implant fixture. The advantage of this single-stage procedure is that the patient may receive a temporary crown right away and the final restoration is completed more quickly. However, this technique is not suitable for all patients.
Oral Hygiene
Oral hygiene is essential. Implants, prostheses, gums and teeth must be meticulously cleaned every day so that they remain free of dental plaque. Attention to oral hygiene will increase the chances of success. Your surgeon, prosthodontist or dentist will give you instructions and reading material regarding oral hygiene. If for some reason you are unable to maintain rigorous cleaning, inform your surgeon, prosthodontist or dentist – as implant hygiene is a life time commitment for the patient and dentist.
After implant surgery
- Rest at home following the surgery.
- Some people require several days off work, school or other activities.
- Do not drink alcohol while taking pain killers or antibiotics.
- Consume soft foods, such as soups, pureed vegetables and meats for the first few days.
- Drink plenty of fluids.
- Ice packs may help reduce swelling and pain.
Success rates
The short and long term success of the implant is determined upon a number of factors, including:
- The health of the jaw bone and its ability to heal well.
- The type of implant.
- The number of implants and the type of prosthesis.
- The position of the implants ie. Upper or lower jaws.
- Your general health.
- The skill of the surgeon.
- If you smoke or have diabetes or take Bisphosphonates/radiotherapy
Approximately 95 in every 100 patients can expect to undergo successful implant treatment. It is difficult to predict how long an implant will work properly in a particular person. Most implants remain in place and function efficiently for ten years and often more. In some people, every implant will be successful, however in other people the implants may not integrate well with the jaw bone. While implants are not successful for everyone, they are effective in most people.
Your surgeon will discuss the potential long term success of implant treatment and the best possible system that will most benefit you.
Possible Side Effects And Complications Of Dental Implants
All types of surgery have potential risks. Complications can sometimes occur despite the highest standard of practice and care. Your surgeon will assess any potential risks that the implants or prostheses may cause to your dental or general health. You will undergo health checks prior to, during treatment and follow up with your surgeon. Should you experience any side effects, this would usually occur within the first 12 months. Serious complications rarely occur after 12 months. If you have a side effect due to the implant, inform you surgeon, prosthodontist or dentist. The following list is intended to inform you about potential problems, not to alarm you. There may be others not listed here.
Short Term Problems
Pain and swelling The degree of pain and swelling near the implant site generally depends upon the number of implants inserted into the jaw. Pain or discomfort and swelling may last for several days. Pain may be minimal in some people and more significant in others. Your surgeon will prescribe pain relief if required. Pain generally begins to diminish after the second day, but some people may require pain relief after one week. If pain does not decrease as the days go by, inform your surgeon.
- Implant failure
One implant or more may fail to integrate properly with the jaw bone. Your surgeon may have to remove the implant and insert another implant in nearby bone. Alternatively, after the failed implant has been removed, another implant may be inserted in the same site after the bone has healed completely. - Speech
Some people may have difficulty with speech following insertion of the prosthesis. This often takes some time to become accustomed to the prosthesis. If the problem is persistent, speech therapy may be required. Some people report improvement in their speech after the prosthesis is fitted. - Gingivitis
Inflammation of the gums is caused by poor oral hygiene, not usually implant surgery. - Perforation of nasal sinus
In some implant cases the tip may be inserted into the nasal sinus floor. This can sometimes cause an infection but can be readily controlled. - Haemorrhage
Life threatening bleeding (haemorrhage) from the floor of the mouth can happen to some patients but it is rare.
Long Term Problems
- Infections
In some instances, an infection may occur around the implant (local)
Infections are treated with antibiotics. If an infection cannot be treated effectively, the dental implant may require removal. Serious infections are generally not related to the implants themselves, but may arise when implants are inserted. Following implant surgery, if you have continuing pain around the implant site/s, have a fever or generally feel unwell, inform your surgeon as soon as possible. - Nerve injury
Implants can push against major nerves in the jaw and bruise them. This can cause numbness, tingling and loss of sensation in the gums, cheeks, lips, chin, tongue and around the upper and lower jaws. In most cases, if a nerve is injured, it will usually heal. Whilst it is healing, numbness, tingling and pain subside. In some people however, complete healing of the nerve may take 6-18 months. In rare cases, the nerve may not heal completely. Rarely, patients have reported chronic pain. Numbness or altered sensation may be permanent and may cause significant discomfort. - Bone loss
In some people, implant treatment may impair bone loss in the area surrounding the implant. - Build up of tissue (hyperplasia)
Gum tissue may increase around the top of the implant where it protrudes through the gums. This is referred to as “hyperplasia” and can be unsightly. The area may be sensitive and inflamed and may require surgery. Inadequate oral hygiene is usually the cause of this problem. - Crown fracture
A part of the prosthesis can fracture or chip. If the problem is serious, a new prosthesis may have to be made and fitted again. - Loose prosthesis
The special screws that fix the abutment to the implant fixture, or the prosthesis to the abutment, may become loose. This may cause the prosthesis to feel loose-fitting. The cause will be investigated and then the screws could be removed, replaced and tightened. - Fracture of the jaw bone
In rare cases, implant surgery can cause a jaw bone to fracture. This can be painful and may require further specialist treatment. - Swallowing an implant component
Small parts of an implant or an instrument can be swallowed or inhaled during surgery. This may occur even though the surgery is carried out with the utmost skill and care. It can result in serious infection and other complications. A procedure may be required to recover the item if inhaled. - Adjacent tooth
In rare cases, a tooth that is adjacent to an implant may be adversely affected and have to undergo root canal treatment. Or more uncommonly, removal of the tooth may be necessary. - Osteonecrosis
- Patients taking bisphosphonates or have had radiotherapy have a greater risk of necrosis of the jaw bone near to the operation site and infection around the implant. This may cause implant failure. Patients planning to have implants and are taking bisphosphonates, should discuss the risks with their surgeon. Patients with implants have a small risk of loss of integration if commenced on bisphosphonate treatment for bone disease at a later stage.
Follow Up
A 1, 3 and 5 year follow up is essential to assess gum health around the implant site and to ascertain whether bone loss is taking place. If this is detected early, very often the condition can be treated and the progression of the bone loss ceased. It is important to ensure that these follow up appointments are scheduled and attended to prevent irretrievable bone loss around the implants.